What is the temporomandibular joint?
It is the joint that connects the lower jaw with the scull. There are two temporomandibular joints, one on each side. The lower jaw is not a real part of the skull, but a separate anatomical entity, which is literally “hanging” from the skull with a set of muscles, tendons and ligaments.
What does dysfunction of the temporomandibular joint mean?
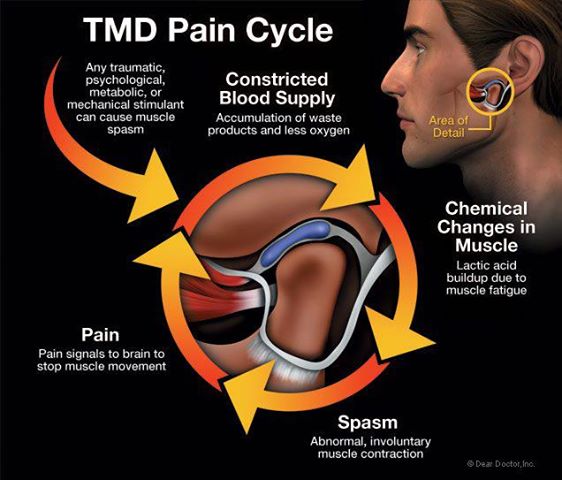
Dysfunction of the temporomandibular structure (TMJ syndrome) is a term used to describe certain disorders in the jaw joints or the muscles controlling their movements.
What are the symptoms of TMJ dysfunction?
The temporomandibular dysfunction can cause the sound to be heard in the joint when the jaw opens and closes, headaches, jaw pain, jaw blocking when the mouth is closed or opened, limited mouth opening, pain in front of the ear, pain that spreads to the shoulders, neck and back, spasm or pain in the muscles used for chewing.
Other symptoms that can be perceived as part of the TMJ syndrome but are actually caused by another condition are: nausea, ear pain, hearing impairment, “noises” in the ears, known as tinnitus, vertigo and blurred vision.
What are the causes of the TMJ dysfunction?
The exact causes of temporomandibular malfunctions are still under discussion. 90% of people with TMJ dysfunction are women of childbearing age. Many times the TMJ is associated with inappropriate activities such as “tightening” or “grinding” the teeth, yawning or laughing with too much mouth open, chewing hard food, chewing gum and so on.
Other causes of dysfunction of the TMJ are the following: abnormal structure of the temporomandibular joint, dental work requiring prolonged and wide opening of the mouth, athletic injuries and injuries from road accidents affecting the chewing muscles, diseases such as osteoarthritis, medical procedures such as intratracheal intubation, tooth loss, incorrect jaw joint, poor tooth dental occlusion and anxiety.
How is diagnosis made?
The results of medical history and physical examination are those that lead to the suspicion of a temporomandibular malfunction. Laboratory tests are often used to rule out other illnesses that cause similar symptoms. Dental radiology can often help with diagnosis.
What is the treatment?
The initial treatment of temporomandibular dysfunctions includes the identification of actions that aggravate the symptoms, such as TMJ control movements, wide mouth opening, tightening and “grinding” the teeth. Many people do not realize that they are doing these things.
Other measures used to treat temporomandibular dysfunctions include the following: hot / cold patches, massage in the TMJ area, anti-inflammatory, muscle relaxant and anxiolytic drugs, physiotherapy, which may include mild jaw exercise, relaxation therapy, small bites that do not include hard foods, avoidance of chewing gum and stress control.
If the above fails, visit a dentist specialized in temporomandibular disorders. In severe cases that do not respond to other therapies, surgery and the use of grafts to replace the joint may become necessary.
What can be prevented?
Preventing temporomandibular disorders is not always possible. However, the following measures may be useful in avoiding or minimizing the symptoms of TMJ syndrome:
Correction of harmful habits, mainly by the use of temporary plastic devices, known as “mouthguards”, to prevent the teeth from “tightening” and “grinding”, avoiding injuries in the TMJ region, restoring missing teeth and correcting dental abnormalities.
What are the long-term results?
Prolonged temporomandibular dysfunctions can lead to joint deformity and to the jaw and tooth disorders. For many people with TMJ syndrome there is no long-term effect, while in other patients the symptoms may be subdued without any treatment.